This paper briefly summarises the discussion of a committee which aimed to assess clinical trials conducted in Guinea, Sierra Leone and Liberia during the 2014-15 Ebola outbreak in West Africa. The committee was established by the United States National Academies of Sciences, Engineering and Medicine. The outbreak highlighted many difficulties in the biomedical research response to major outbreaks, and commentators disagreed over a number of topics. High on this list was the ethical implications of using randomized controlled trials (RCTs) for vaccine and therapeutic development in an outbreak situation.
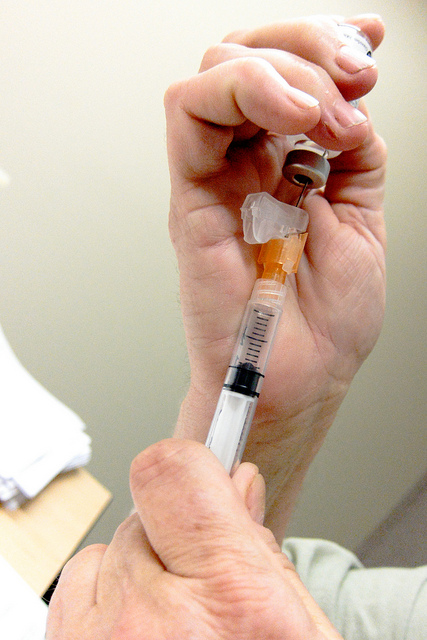
Image: Daniel Paquet | Flickr
The committee reached four major conclusions:
-
Research is an essential component of epidemic response. For certain diseases such as Ebola, where animal models are unreliable, outbreaks offer the only opportunity for the efficacy of treatments to be tested.
-
RCTs are the most reliable way of identifying benefits and risks of interventions. The committee argued that every effort should be made to implement RCTs during epidemics, except in rare circumstances.
-
The committee rejected the view that RCTs were unethical during the Ebola outbreak, put forward by some stakeholders. Proponents of this view argue that clinical equipoise (the belief that no intervention is ‘better’ than another) cannot be achieved in outbreak scenarios. However, the committee disputed this, as there is no way of knowing whether an intervention will be better than the current standard of care that the control group receive. They further argued that, some interventions might even worsen patient health.
-
Effective engagement and communication of reliable scientific information is vital for trials to take place in epidemics. During public health emergencies, there are heightened levels of distrust and uncertainty. Rumours, such as the idea that treatments were ‘secret serums’, were linked to resistance to randomized trials in some regions. However, in communities where good engagement with research had been achieved, randomized trials went ahead successfully. The committee argued that this demonstrates the value of good engagement in epidemic situations. They argued that this engagement must occur in interepidemic times to ensure readiness of the communities.
Read the summary paper here, or purchase the full report here.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Please Sign in (or Register) to view further.